New York State
Public health experts’ prescription to fight the coronavirus
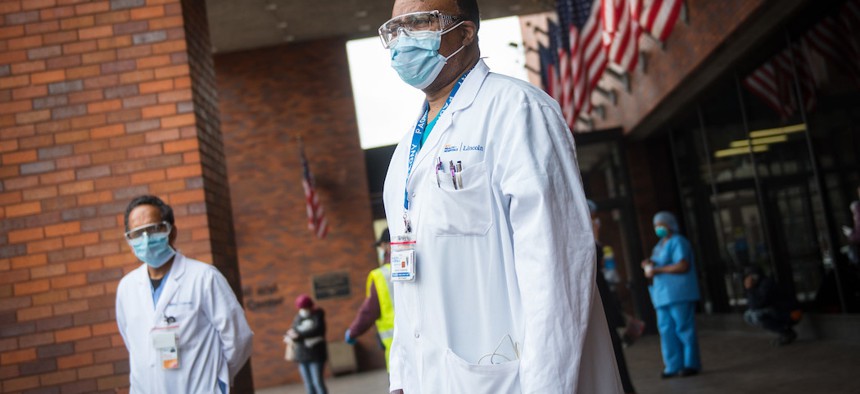
Healthcare workers outside of NYC Health + Hospitals/Lincoln in the bronx on April 8th. Michael Appleton/Mayoral Photography Office
On Jan. 22, Netflix released the six-part docuseries “Pandemic: How to Prevent an Outbreak,” which prominently featured Dr. Syra Madad, a top public health official with New York City Health + Hospitals. “It’s just a matter of time where the next pandemic is going to start,” Madad, who is responsible for preventing outbreaks in the city’s public hospitals, says early on in the first episode. “We just don’t know where or how, but we know it will.”
Madad’s remark proved eerily prescient. By the beginning of March, the first novel coronavirus case was identified in New York City, which quickly became the epicenter of a growing pandemic in the United States. And while politicians have suggested in recent days that restrictions on social interaction in New York and elsewhere have helped turn a corner in the public health response to COVID-19, Madad and other experts warn that there’s still much more to be done – and much more to be learned about how the virus.
In City & State’s latest webinar on the coronavirus response, Madad, the senior director of the System-wide Special Pathogens Program at Health + Hospitals, was joined by Dr. Saskia Popescu, an infectious disease epidemiologist and infection preventionist. The medical professionals made a presentation on how outbreaks like SARS and MERS have informed current epidemiological efforts, where the United States’ public health response fell short, and what should be done going forward. Madad and Popescu also took questions from CIty & State and audience members about whether New York has actually reached a peak, the importance of increased testing and contact tracing, and the perennial lack of federal funding for public health. The transcript below has been edited for length and clarity.
Click play on the video below to watch the webinar.
City & State: What are the models showing us right now, both in New York and nationally? Is it possible to tell if we’ve reached the peak? Is the curve flattening?
Dr. Popescu: I think the hard part with models is you have to take them with a little bit of a grain of salt. Epidemiological models are based on forecasting. They're not predictions, so this is going to change every single day as we get more cases in, as we're learning where that curve is going. I do stress the importance when people who are looking at them, how many variables are the models accounting for? And not to get so set on a date. I've personally seen that where I've had administrators say, “Well, the peak in Arizona is going to be at this time.” We know that can change, and the truth is that it takes at least a couple of weeks to see if our current efforts are going to work appropriately and help decrease the case counts. When we start to “open things back up,” you're going to see a rapid spike. It's much faster to see that kind of change when cases increase. We have to be mindful when it comes to cases. A lot of states are plateauing, some are increasing, some are decreasing. It's very challenging right now, when you're looking at preparedness across a nation and if we can relax those kinds of restrictions when we're all in different situations and the models that we are using for forecasting are constantly changing.
City & State: What do we know about people who have already had COVID-19 and recovered? Could they get sick again? Could they still spread germs?
Dr. Popescu: I think we are still learning a lot about the status of immunity and serology testing. The CDC guidance has been quite helpful in terms of seven days following your positive lab results or 72 hours after the resolution of symptoms without a fever. Again, this is still a very novel disease. We're still learning a lot about it. I hate to give any cement answer.
Dr. Madad: I think what she stated is obviously very accurate. Right now, we still do not know a whole lot about this disease in terms of how long the immunity can last for if you do get infected. One of the things I'll mention is there's a difference between reading an article, a report, or, obviously, a scientific study. There are a lot of articles out there that have talked about people getting reinfected with COVID-19 that didn't have immunity. But please again make sure you go to a credible source. These are reports. These are people that have no scientific background, and they're writing these articles based on information they may have received. These are not scientific studies that have a cohort of individuals that are studied over a period of time to look at the reinfection rate and how long immunity can last for. That information is not available yet. Again, this virus is only four months old. We're learning every day. But you know right now that's a question that will hopefully be answered in the very near future.
Dr. Popescu: I'd like to mirror that. I think part of the problem too is we are so inundated with information. People are reading a lot about a single case, or they’re seeing preprints. This is definitely a big issue right now. When you are reading, whether it's the news or things that are coming out of a study that has just been done, really look at the number of people that were studied. If this is a preprint, has this gone through peer review? Because a lot of the research that's being done right now is happening very, very fast and we need to be mindful of the information and the science communication that is coming out to you. I saw this with the concerns for aerosolization in airborne. The truth is many of the nuances of studies aren't necessarily real world or they're very isolated events. So when you're reading this, as Dr. Madad noted, be mindful of what you're reading, who you're reading it from. Is this person an expert on it, was this a study or are you reading it thirdhand? It's easy to get a lot of fear or the sensationalism out of what's being shared right now.
City & State: Just this week, the de Blasio administration said it is taking steps to obtain and manufacture a significant amount of test kits. Does this mean the city can lift restrictions on social distancing, or are there other factors to consider?
Dr. Madad: Testing is certainly one very, very large aspect, and we're certainly moving in the right direction. It's great that we're able to afford the test kits that are needed. But obviously, there are other factors that go into play when we talk about lifting restrictions. Mayor de Blasio has done a wonderful job outlining some of these other factors that we're looking at. He called them indicators or clues. So testing is one of them, but also looking at the number of hospital admissions, people in ICU and things like that. So it's a number of different things that go into lifting these types of restrictions.
City & State: Both on the national level and here in New York, how are we doing in terms of protecting health care workers, from training to supplies?
Dr. Madad: This type of situation that we're in requires coordination, collaboration and communication from the local, state and federal level. We are seeing this play out very much so. This is something that requires an all hands-on deck approach. When we're talking about more equipment and supplies, a lot of different levels of government are working together to get the necessary equipment and supplies that’s needed. In a health care delivery environment, our timeline is hours, days and weeks. Right now, certainly, we have the resources that we need, but we know that this epidemic, we're in it for the long run. So we need to continue to have injections of these equipment and supplies to maintain them at a par level. That's why we need to continue to advocate for more.
City & State: I also wanted to go deeper on contact tracing. My understanding is that we were way behind from the get-go, especially compared to other countries. What difference does having enough contact detectives make?
Dr. Popescu: Contract tracing is a cornerstone in epidemiology and I really think our ability to do it is very representative of the public public health system we have and how well we're supporting it. So that means, from the beginning I think a lot of us have been saying we need to do better in terms of public health resources. If you can't do contact tracing in the very beginning, that's a pretty big indicator that your health departments are already struggling. So now when they're inundated, that means that we really can't do it. And the truth is that to kind of start relaxing some of these restrictions, we have to be able to do contact tracing because that allows us to not only identify a case, which is where that rapid diagnostic comes into play, but make sure that they're isolated appropriately and evaluate any close contacts they had within their period of potential infectiousness and get them to quarantine or make sure we're kind of communicating with them: “Hey, you might be at an increased risk for acquiring this disease, please stay home.” And our ability to do that is huge. That means we can help control the outbreak and help break that chain of transmission. So when we're not able to do it, that really prevents us from getting involved and disrupting the chain of transmission. I think that's hard, because it's very telling of a public health infrastructure and the resources it has.
Dr. Madad: One of the biggest issues we have been facing, not just from a public health standpoint but also from the health care delivery standpoint is the cuts to funding at the federal level. Many of you may be familiar with the Hospital Preparedness Program and the PCP, the Public Health Emergency Preparedness Program, both funded you know at the federal level. Both of these programs have continuously taken very large cuts in terms of funding capacity over the years. In fact, when we talk about HPP, the Hospital Preparedness Program, this is the money that from a hospital standpoint we use to maintain that state of readiness. This is the money that we use to do our drills and exercises, and continuously train our staff. This continues to dwindle down. So if you look at the Hospital Preparedness funding that has been allocated for, you know, this year and future years, it's really at an all-time low. I mean it's extremely unfortunate. And the approach that we've always had here in the United States is a very unfortunate approach from a federal standpoint. What this means is that when we have an epidemic they inject millions of dollars for that specific epidemic and then once it's over that funding is taken away that staff is basically, is let go, if you will, or repurposed, and the expertise that was built for that that particular situation that can be extrapolated for many different situations obviously doesn't exist. Case in point, the Netflix docuseries, one of the things that I highlighted, and even at the end when you see me doing that Ebola exercise at Coney Island hospital and I'm talking about the funding, the funding I'm thinking about is the Regional Ebola Special Pathogen Treatment Network. Millions of dollars were allocated in 2014, but it’s an entire network of frontline hospitals. We have 6,000 hospitals in the United States. When we talk about the regional Ebola Special Pathogen Treatment Center that was established, you have frontline hospitals, assessment hospitals, Ebola treatment centers, and regional Ebola treatment centers. And Congress has now finally only approved funding for 10 regional centers, so these are only 10 hospitals. Now if you talk about COVID-19, this is again an all-hands-on-deck approach. Every single hospital plays a role in this. And so all those frontline hospitals, those 6,000 frontline hospitals, they're not getting any funding. So that's funding that’s unfortunately set to expire this month and there's no indication from Congress that that that work is going to be renewed besides the 10 regional centers. So that shows you a huge problem in our approach to infectious disease preparedness and how we need to continue to prepare and invest in preparedness dollars. And that's not the case right now, and so we really need to have a different approach moving forward.
Dr. Popescu: Coupling in on that too, we also have, as Dr. Madad noted, funding for those 10 regional centers, but for the rest of the thousands of hospitals that exist there's really no incentive for hospitals to invest in these costly prevention efforts and preparedness efforts, unless you have hospital administrators that opt to invest in them. There's no requirement. There are emergency preparedness rules through Medicare, but unfortunately they're not specific to infectious diseases. So I think that's a huge gap and whether we're looking at it from a national level or even your local hospital, unless they decide to put money into this there's no priority for it, there's no federal mandate.
City & State: We talked about the federal aspect here, but what city or state policies need to change?
Dr. Popescu: I think we definitely need to need to put more money into public health, because hospitals work very closely with our state and local health departments to ensure readiness, but if we're all in the process of getting funding whenever an outbreak or a pandemic occurs, it's going to be dwindling. So my concern is there's just not enough resources for local hospital coalitions or the HPP to really be focusing on that and then also bringing in the public health department to collaborate with multiple hospitals in the areas.
City & State: For those of us who are not medical professionals or scientists, what are the reliable sources we can turn to that do accurate reporting?
Dr. Popescu: I always like to encourage people, if you are following someone on social media, look at their background. Look at who shares their information because most of us in the fields all know each other and we share each other's names. We encourage each other. So I think that's always a red flag, if they're kind of on their own, look at their backgrounds. But, you know there's so many great resources. Stat News is really wonderful. Ed Young has been really great with The Atlantic, But, also Scientific American, the CDC, the WHO, those are your steadfast sources that you want to stick to. But, I think it's very easy to see sensationalism. I personally stick to the CDC and the WHO, and then I follow my trusted resources, Dr Madad being one of them, but my biologists, my stats people, all of them, because I know that they're experts in their field and they're going to review the information before they share it.
Dr. Madad: And just to add to that, you know, I think also at the local level, here in New York City, another great resource that we have is your public health department. So for example, New York’s Department of Health and Mental Hygiene. They are really one of the best in the world. We have one of the best public health departments. And we have an amazing leadership that oversees the Department of Health, and they keep a very robust and up to date website of not only the number of cases we have for COVID, but also additional recommendations and suggestions. One of the things that we know for COVID-19 is that the response at the local level differs from state to state. And so some of the regulations and guidance may be different for New York City versus something that's happening for example in California or Utah. So just make sure that you know who your public health department is and and reach out to them if you have any questions or concerns, but also look at their website and see what type of information that they have, because I know from a city department of health standpoint, we rely on them very heavily on a number of different things and they have been amazing partners throughout this whole thing.
Dr. Popescu: Ithink also the Johns Hopkins Center for Health Security has been really wonderful at sharing information, but also their GIS maps.
City & State: Is there any indication that there may have been cases in New York City as early as December? Will we ever know how early a case came to New York?
Dr. Madad: So, we know one of the testing that's going to be up and running hopefully soon as you know is the serology testing to see who's immune. But, we can also do some genetic analysis and look at the footprint of the virus. But it's still very hard to tell when the virus obviously first started here in New York City or New York state. We were essentially, at a national standpoint, blinded to you know, when this epidemic started here and how many cases we had early on and even now, because of the whole testing fiasco. So it’s something that we'll probably learn more about as this epidemic continues and a lot more people look into this and investigate when a patient zero first arrived here in New York City and in New York state but right now I think that's something that is to be determined.
Dr. Popescu: I also think that's a really great reason to invest in public health because it's your epis that are going to be doing that epigenetics investigation. And so another reason why we want to really increase public health funding and support for this is because they'll ultimately be doing that and helping us identify some of the gaps that were very prevalent in the beginning and how we can fix those for the future.
City & State: With the news that COVID-19 can linger in the air, what are your recommendations for elevators and also for air ducts and apartment built buildings? Should people seal the vents?
Dr. Popescu: The airborne question is one that I think we've all heard so many times. The truth is that we're still learning so much about how long things are lingering on surfaces. But droplet transmission they tend to kind of hover in the air and then they fall, and as long as you have an HVAC system and air circulation that's definitely going to help. Obviously if you're trapped in an elevator with someone who's coughing a lot, that's not ideal, and that's why mask wearing can be helpful, because it really is about containing the microbes that somebody is coughing out. But I wouldn't suggest taping off air ducts because you want air circulation, you want the HVAC system and the heavy filtration to be working, and if you take those off they won't and we need that we want that, so I wouldn't encourage that. It’s hard to maintain social distancing in elevators. That's why the community masks wearing is encouraged for that situation especially. Hand hygiene really goes a long way. If somebody is coughing and you're in an elevator, get off the elevator or ask them to maybe cover their cough, but please don't cover your vents. And, most of us, we're very fortunate where we have HVAC systems that constantly are recirculating the air, so I'm not as worried about that. It's more in a closed environment with no air circulation for a prolonged period of time that I would worry about.
Dr. Madad: Obviously, the elevator is a certain situation that you're in, but this is why you know the recommendation is to keep that six feet distance. Many of you may have seen an image of somebody coughing or sneezing and you see those viral particles that people are spewing out. These are respiratory droplets and they don't travel extremely far in that sense. And so this is why we want to make sure that you keep that six feet distance to not inhale those particles or if you're around those surfaces you don't touch those surfaces. And all of this makes sense if you look at the whole epidemiology of transmission of viruses and when I talk about COVID-19 still a lot for us to still learn and new information is still coming out every day. But, we know we can rely on at least the foundation and backbone of what we know based on other viruses and the mode of transmission and just general respiratory viruses in general.
City & State: Dr. Madad, you've talked about watching the 1995 film “Outbreak” as a turning point for your career. What did it get right? What did it get wrong?
Dr. Madad: You know with these Hollywood movies, this is something that obviously as I was growing up I used to love watching and I used to love reading about these things. “Outbreak” was one of the movies that got me interested to pursue the career that I'm in. You know, with all of these types of Hollywood blockbusters, there is some truth to it but largely it's sensationalized. But, when we talk about the fear that is generated, and we talk about you know the chaos, and what we know and what we don't know, a lot of that is true and that we're living through right now with COVID-19. You're seeing obviously the effect that it's having not just on individuals, but it's also having a large effect on the economy and society in general. You see, obviously, how many different agencies are playing a part in the epidemic response. It's not just public health departments, it's at the federal level, at the state level, at the local level. And you're also seeing a number of people come together to respond to this incident, so a lot of that is depicted in these movies. But a lot of it's also sensationalized. And it's hard to see what is true and what is not. But, you know, there is some truth to it.
Dr. Popescu: I agree that the chaos that it causes is an important component to this. But every one of these movies does sensationalize, like the whole scene with it going airborne, we know that's not how viruses work. Just take it with a grain of salt and that it is a movie. But, the most important thing again is getting information from the right sources.
Popescu & Madad Hospital Biopreparedness Presentation by City & State NY on Scribd

NEXT STORY: The latest on COVID-19 in Queens