Policy
Health care providers discuss the future of value-based care
City & State's “Innovations in Value-Based Care” conference featured industry professionals who stressed the importance of reducing health inequities among vulnerable populations.
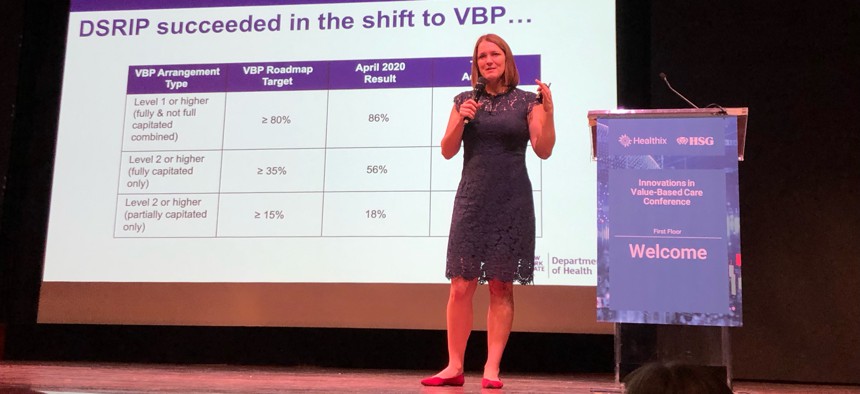
Amanda Lothrop, Medicaid chief operating officer at the state Department of Health speaks to attendees at Healthix’s “Innovations in Value-Based Care” conference on Wednesday. Image by Phenix Kim
Despite the challenges brought about by the COVID-19 pandemic, New York state remains the nation’s leader in value-based care and payment systems. Helgerson Solutions Group CEO Jason Helgerson underlined the importance of value-based care at City & State's "Innovations in Value-Based Care” conference, hosted by Helgerson Solutions Group and Healthix at the Museum of Jewish Heritage on Wednesday.
“I've often said that value-based care is really a social movement. It's about fundamentally improving the lives of individuals, particularly in the case of the Medicaid population, the most vulnerable, in our community, in our society. Whether you're a governmental agency, or community-based organization, or health care or behavioral health provider or a pair, you all have seats at the table when it comes to making the world a better place,” Helgerson said.
Keynote speaker Amanda Lothrop, Medicaid chief operating officer of the state Department of Health, highlighted key elements of the state’s anticipated value-based payment program in addition to what’s expected of the 1115 Medicaid waiver: from specified data collection methods, social care networks and the implementation of both CMMI and CMMI primary care models.
Regarding the use of data collection to reduce health inequities, one of the solutions championed by Lothrop entailed tightening population targets within existing models.
“What would happen if you looked at those local targets and instead started to divide it up by population? So stratify your population to look at the most vulnerable, where is there the biggest gap in your quality measures?” she asked. “If we focus on the average, we leave patients behind.”
According to Lothrop, this focus on specific populations and refining data collection measures will help locate areas of funding and additional investment. Lothrop continued that these specific data collection methods are anticipated in the state Department of Health’s “Value Based Payment roadmap,” which will address different gaps in the existing system.
“We are making an effort with the refresh to focus on a wide range of things. Some of it will be more administrative: how do we consider balancing the needs of providers to look at things like standardizing data or standardizing contract terms such as attribution or target element and cure that with the need to drive innovation and really strike that balance?” Lothrop asked.
One of the key components of the roadmap, in line with the expectations of the 1115 Medicaid waiver, were increased social care networks.
“As we move ahead to the 1115 waiver being implemented in the Medicaid program, we'll be establishing social care networks – these social care networks will be one network per region. The social care networks job is to make the lives of providers and CEOs as easy as possible to get the members the interventions they need. This organization will be found in VBP from the start, they'll be driven in a model that from onset will encourage the mindset of value-based payment to encourage those close lasting relationships,” Lothrop said.
These social care networks will also help facilitate eligibility discriminations, from determining health related social needs and services based on clinical data, in order to base referrals. Lothrop highlighted the holistic impact of social care networks, which will help actively address members’ social care needs to ultimately reduce clinical burdens.
Additionally, the “VDP roadmap refresh” intends to build on its existing innovator program, along with the implementation of CMMI and CMMI primary care innovation models, of which New York is the only state to implement both.
“There will be the CMMI models that we've talked about. In primary care, there is the head model, which was just announced a few weeks ago, this (CMMI) is a model that we're exploring for downstate New York. This model will be the foundation of the global budget models that you've seen. The difference here is, one, CMMI is leaning a lot of flexibility to the state, so we'll be able to shape this to what we collectively need it to be. And two, will be paired with a really heavy primary care investment,” Lothrop said.
Lothrop also emphasized the importance of prioritizing primary physical care, whose effects ripples across all sectors, from behavior health to one’s social well-being:
“With that, we also recognize that primary care is critical to moving the needle statewide. That's the foundation in value-based care. So if you pair health related social needs with primary care – we're going to have progress. Nationwide in 2020, we as a country spent 12% of our health care funding on primary care, New York that was closer to 8%. And that's not enough, we know that that's where the change happens. We know that that's what numbers need to be successful.”
Yet in order to actualize better results, New York’s success in robust value-based health care ultimately lies in effective partnerships and collaborations.
“If we are to implement a successful value-based approach in healthcare, let's not forget how important it is to come together as a community as partners to achieve this balance between high-quality care and cost containment. Keeping our care patient centered, collaborative and transparent. It's a team effort, a community effort in delivering equitable patient care and access and reducing health disparities, right here at home”, said Todd Rogow, CEO of Healthix.
To deliver value based care, there will be a call for value based physicians. A discussion on a panel entitled “Physician Engagement in Value-based Arrangements,” focused on how physician engagement looks in value based care arrangements and how the profession should be poised for the future.
“The COVID-19 pandemic revealed cracks in our health system that community doctors who serve the underserved have long known. Why are our patients sicker? What are the effects of the social determinants of health, like housing nutrition, education and behavioral health? What role do equity and access play?” asked Nick Youngstrom, CFO of SOMOS Innovation, who participated on the panel. “So, as we recover long-term, how can we reform and improve? Preventive care supported by value based payments is an answer and must be a strong part of the equation going forward and deserves its growing recognition.”
“Moving from the fee-for-service model to one that revolves around the total health of the patient – especially patients from lower-income communities – is revolutionary,” Youngstrom added. “It’s transformative. It’s finally a provider-led, community-based, patient-centered, 360-degree long-term intervention that’s overdue and focuses on a system that keeps patients well instead of waiting until they get sick. As community providers, we strongly support the Governor in her call for a new waiver to facilitate this work long-term. Value Based Payments are the future of care.”

